Exercise improves mood, cuts anxiety, and lifts daily function, say nursing journals.
If you care for people with mental health needs, you’ll see this every week. Exercise is a simple tool that fits into care plans and real life. In this guide, I unpack exercise for mental health nursing journal articles with clear steps, doses, and tips. I’ll share what works, where it fails, and how nurses can use it today. You’ll get a practical map built on research and bedside experience.
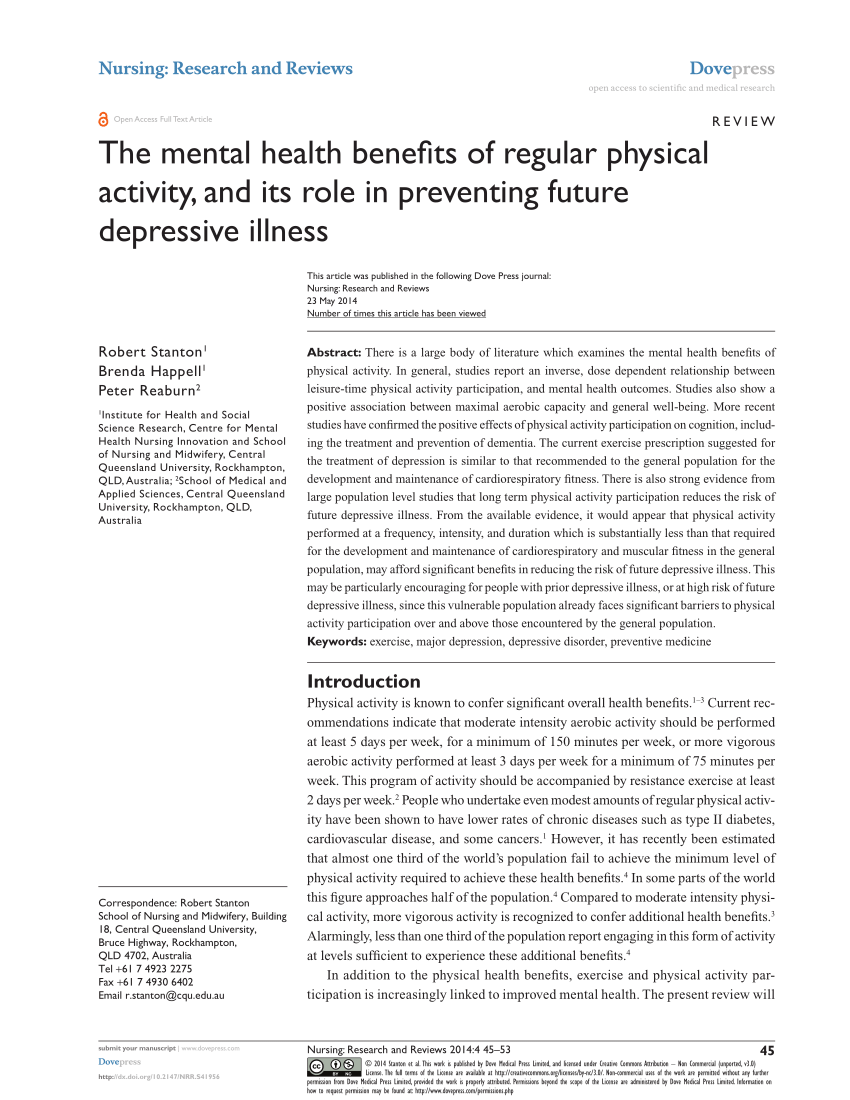
What the research shows at a glance
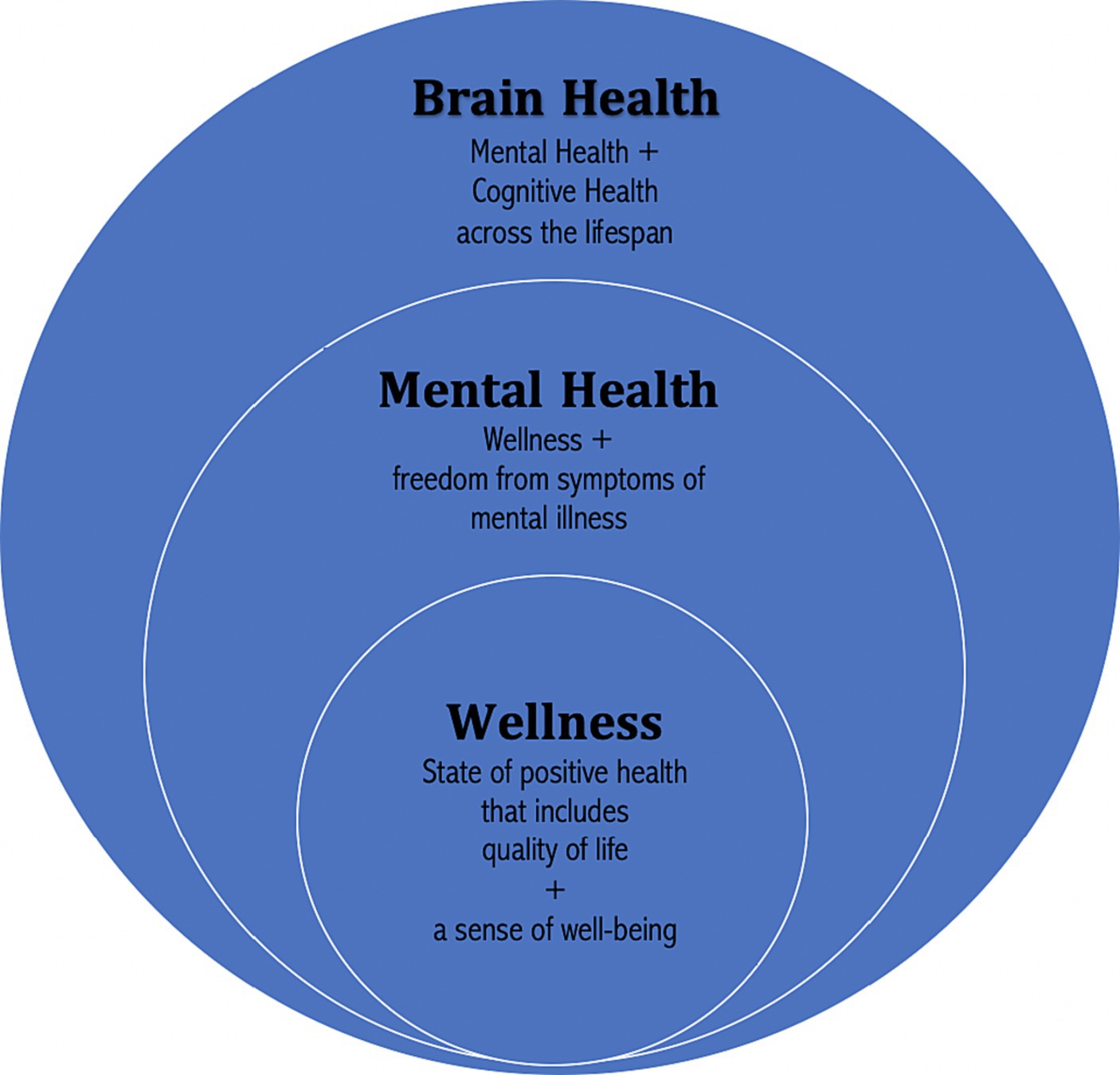
Most mental health nursing journals now agree on one core idea. Exercise helps the mind, not just the body. Trials and reviews keep finding the same thing across settings.
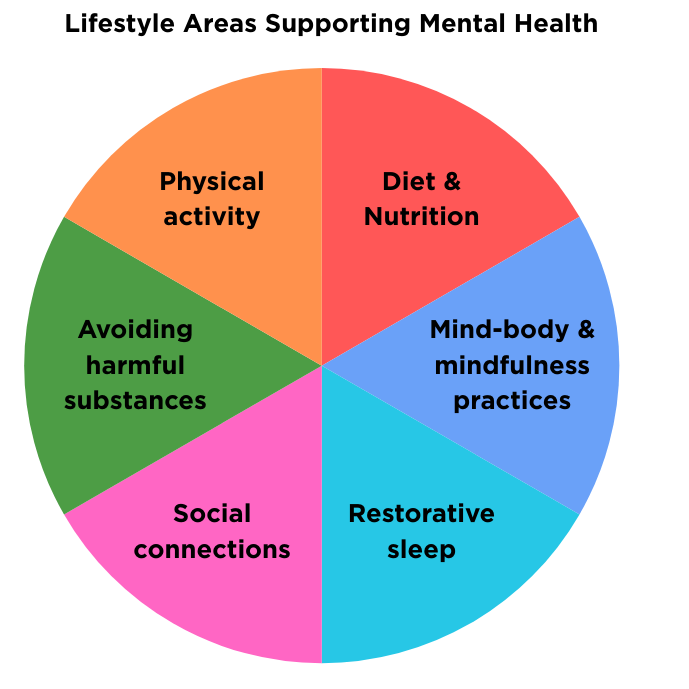
- Depression. Regular aerobic or strength work reduces symptoms to a meaningful level.
- Anxiety. Exercise calms the system and improves sleep and worry control.
- Serious mental illness. Walking groups and strength plans boost mood, energy, and social ties.
- Trauma and stress. Mind–body work like yoga or tai chi reduces arousal and improves sleep.
- Cognition. Movement helps focus, memory, and speed, especially with structured plans.
These gains do not need elite workouts. Think brisk walks, light weights, short circuits, or chair-based moves. Across exercise for mental health nursing journal articles, three to five sessions per week show the best results. A common target is 150 minutes of moderate work each week. Many patients improve even with less at first.
In my practice, the best outcomes came from simple routines. We tracked mood, sleep, and steps. The trend was clear within four weeks. Exercise for mental health nursing journal articles mirrors that pattern.
Why this matters in day-to-day nursing
Exercise is low cost, flexible, and safe with good screening. It can be done in a room, a hallway, a park, or a gym. It supports medications and therapy. It gives patients a sense of control and a quick win.
From the floor, I learned one key lesson. Most patients do not need a perfect plan. They need a plan they can start today. That theme repeats across exercise for mental health nursing journal articles. Small steps beat big promises.
- It reduces side effects from some drugs, like weight gain and fatigue.
- It improves sleep, which helps mood, pain, and coping.
- It builds routine, which is vital for relapse prevention.
When nurses lead the way, teams follow. We can screen, set goals, coach, and track outcomes. We can also link to community resources.

Exercise types and doses that work
Use clear, simple choices. Let patients pick from a short menu. Then set easy doses and build up. This is a top tip in many exercise for mental health nursing journal articles.
-
For depression
- Brisk walking, cycling, or light jogging.
- Dose: 30 minutes, 3 to 5 days per week.
- Add strength work twice a week for extra gain.
-
For anxiety and sleep
- Walking, yoga, tai chi, or swimming.
- Dose: 20 to 40 minutes, most days.
- Add slow breathing at the end.
-
For serious mental illness
– Group walks, circuit stations, or chair-based strength.- Dose: 20 to 30 minutes, 3 days per week to start.
- Focus on fun and social contact.
-
For bipolar disorder
- Use moderate intensity and regular timing.
- Dose: 20 to 40 minutes, 3 to 4 days per week.
- Avoid late-night high-intensity work.
-
For trauma recovery
- Mind–body work, gentle strength, and steady walks.
- Dose: 20 to 30 minutes, 3 days per week.
- Keep choice and control with the patient.
A common pattern in exercise for mental health nursing journal articles is “start low, go slow.” Raise time by 5 to 10 minutes every one to two weeks. Keep rest days.
Step-by-step nursing protocol to start today
Here is a simple, safe flow you can use. It fits most settings and mirrors what you will see in exercise for mental health nursing journal articles.
- Screen basics. Check vitals, falls risk, pain, and cardiac history.
- Ask goals. Mood, sleep, weight, energy, or social links.
- Pick one activity. Aim for what the patient likes or can access.
- Set a tiny first step. For example, a 10-minute walk after breakfast.
- Set a SMART goal. Clear, short, doable, and tracked.
- Plan the week. Put sessions on the calendar like meds.
- Teach safety. Warm-up, cool-down, and when to stop.
- Track outcomes. Mood scale, sleep log, and steps.
- Review weekly. Keep what works. Trim what does not.
- Link supports. Peer groups, apps, or community classes.
Use simple tools. A paper log, a phone timer, or a step counter. In my charts, the best predictor of success was a plan tied to a time and place. Exercise for mental health nursing journal articles also note this habit cue effect.

Safety, contraindications, and risk checks
Exercise is safe for most patients when we screen first. Look for red flags and set clear rules. This is a core theme across exercise for mental health nursing journal articles.
- Check meds. Some drugs change heart rate, blood pressure, or heat tolerance.
- Watch for dizziness, chest pain, severe shortness of breath, or fainting.
- Review falls risk, foot care, and hydration.
- For psychosis, avoid crowded or over-stimulating spaces early on.
- For bipolar disorder, avoid sleep loss from late sessions.
- For acute crises or high suicide risk, use supervised sessions.
Simple screen tools help. Ask about heart disease, chest pain, and fainting. Check blood pressure and resting heart rate. Start with short, low-intensity bouts if unsure. Document consent and teaching.
Measuring outcomes and documenting progress
What gets measured gets managed. Use brief tools. Keep it light and fast. Journals value clear outcomes, and so do patients.
- Mood and anxiety
- PHQ-9, GAD-7, WHO-5, or a simple 0–10 mood scale.
- Sleep
- Sleep diary or a short sleep survey.
- Function and fitness
- 6-minute walk test, step count, or stairs climbed.
- Metabolic health
- Weight, waist size, blood pressure, glucose, and lipids.
- Adherence
- Sessions done this week and minutes per session.
- Patient voice
- One sentence each week: “What changed for you?”
Log data every one to two weeks. Share graphs with the patient. This boosts buy-in and helps the team. It also aligns with many exercise for mental health nursing journal articles that stress patient-centered tracking.

How to read and use exercise for mental health nursing journal articles
A quick method helps you sort signal from noise. Here is the way I teach new staff.
- Define your PICO
- Patient, Intervention, Comparison, Outcome.
- Search smart
- Use CINAHL, PubMed, and PsycINFO.
- Pair terms like exercise, physical activity, mental health nursing, and outcome names.
- Appraise fast
- Look at sample size, randomization, and blinding.
- Check adherence, intensity, and how outcomes were measured.
- Apply with care
- Match the population and setting to your patient.
- Use the same dose, if safe, for two to four weeks before judging.
Keep a one-page summary of your top five papers. Note the dose, effect, and limits. This habit is common in strong teams and seen in exercise for mental health nursing journal articles on implementation.
Real cases and lessons learned
Case 1. A 42-year-old with major depression started 10-minute walks after lunch. She built to 30 minutes, 5 days a week over six weeks. Her PHQ-9 dropped by half. The key was pairing the walk with a set meal time.
Case 2. A 29-year-old with psychosis joined a staff-led hall circuit three days a week. Sessions were 20 minutes with music and light strength. Negative symptoms eased, and he joined a community group after discharge.
Case 3. A 55-year-old with anxiety and poor sleep tried evening yoga. Sleep improved but he felt wired at night. We moved sessions to mornings. Sleep and daytime calm improved within a week.
These cases show the main point in exercise for mental health nursing journal articles. Dose, timing, and patient choice matter as much as the activity itself.
Frequently Asked Questions of exercise for mental health nursing journal articles
What is the best first step for a new patient?
Start with a 10-minute walk, three days this week. Keep it the same time each day to build a habit.
How fast should we expect mental health changes?
Many patients feel a lift within two weeks. Larger gains often show by week four to six with steady practice.
Do we need a gym for this to work?
No. Halls, parks, stairs, and living rooms are fine. Bodyweight moves and walks cover most needs.
Is strength training as good as cardio?
Yes, for many patients. Strength work two days a week helps mood, sleep, and function.
How do I keep patients engaged?
Use small goals and weekly wins. Track progress, celebrate effort, and keep choices simple.
What if the patient has chronic pain?
Use gentle, low-impact choices and short bouts. Build tolerance slowly and avoid pain spikes.
Can we use apps or wearables?
Yes, if they help, not stress. Step counts and timers support routine and feedback.
Conclusion
Exercise is a proven, flexible tool for mental health care. Small, steady steps change mood, sleep, and daily life. Nurses can lead this work with simple screens, clear goals, and light tracking.
Pick one action now. Plan a 10-minute walk for your next patient and log the result. If you want more on exercise for mental health nursing journal articles, subscribe, share your experience, or leave a question below.




